This section of the website aims to cover topics at the level that could come up in either the MRCGP exam (UK), MICGP exam (Ireland) for GPs and hopefully the MRCP for non-consultant hospital doctors.
Please contact me if you can identify anything else useful that I could add.
Topics covered in order:
Video 1: Psoriasis to TEN
Video 2: Henoch-Schonlein purpura to Pretibial Myxoedema
Vid 4: Other tumours- neurofibromatosis
PSORIASIS
Affects 1-3% population
Peak onsets 15-25 years and 50-60 years
Characterized by abnormally excessive and rapid growth of cells in the epidermis called keratinocytes which go through a much quicker lifecycle then usual
The underlying pathology is complex but in part due to immune dysregulation (different profile of immune cells and cytokines in skin)
Psoriatic arthritis in up to 40%- inflammatory type of arthritis. DRAMA
DIP joints affected
Rheumatoid-like arthtirtis
Asymmetric oligoarthritis
arthritis Mutilans
Ankylosing spondylitis like arhritis
Often have nail changes also (pitting - small pinprick holes, onycholysis - separation of nail plate from nail bed)
Courtesy Dr. Ian McColl
Chronic plaque psoriasis
Characterised by pink red (‘salmon pink”)hyperkeratotic plaques which often occur on extensor surfaces such as knees and elbows
Other areas that may provide clues it is psoriasis: natal cleft, behind ears, umbilicus, nape of the neck, the scalp and the hands/feet
New plaques may occur at areas of skin trauma (kobnerisation)
Guttate psoriasis: (guttate is latin for “raindrop”)
Follows URTI.
Symptoms:
Rash appears around 2 weeks after infection and it appears very acutely with multiple papules/small plaques appearing within a very short time
Palms and soles are usually spared and the diagnosis is a clinical one
Treatment:
Usually resolves over course of a few weeks.
Simple emollients (moisturisers)
For resistant causes: topical steroids or phototherapy (narrow band uvb - come in to clinic about 3 times per week for a period of about 8-10 weeks)
Pustular psoriasis
Can be generalized and this is a dermatology emergency
Get a widespread erythematous rash with pustule throughout it
Patient can be very unwell with fevers, elevated inflammatory markers, tachycardia, dehydration and electrolyte abnormalities
Patient should be admitted if have this for stabilisation of skin and may need to commence a systemic agent
Certain triggering factors can cause this:
Sudden withdrawal of steroids
Infection
Pregnancy
Generalised pustular psoriasis
Localised palmoplantar pustulosis:
A chronic pustular condition affecting the palms and soles
It is a localised variant of psoraisis (about 1/4 of patients will have psoraisis elsewhere)
Almost exclusively seen in smokers
Pustules are superficial and dry out leaving a brown adherent scale which peels off
Palmoplantar pustolosis: actually now considered a distinct entity from psoriasis
Globalskinatlas
Erythrodermic psoriasis:
Erythroderma means widespread erythema of the skin with >90% body surface area affected
This is just one of the caues of erythroderma
May or may not be preceded by usual type psoriasis
Patient can be quite stable with this or can be systemically unwell
Erythrodermic psoriasis. Silvery scale would lead to suspicion of psoriasis.
Flare ups of psoriaiss can be due to – streptococcal sore throat, trauma (koebner phenomenon), beta blockers, antimalarials, lithium
Treatment psoriasis:
Mild to moderate disease:
Topical steroids
Topical calcipotriol (vit D derivative) - eg calcipotriol (dovonex)
Often use a combination strong steroid and calcipotriol (Dovobet, Enstilar foam)
Phototherapy - narrowband uvb safer long term than pUVA so would be first choice
With more severe disease systemic treatment - eg significant body surface area affected, psoriasis in particularly troublesome areas (eg face, hands, scalp, genitals) or if it is significantly affecting the patient’s quality of life
Systemic agents:
Methotrexate
Cyclosporin
Others - Acitretin (a retinoid much like roaccutane), Apremilast, Fumaric acid Esters
Biological immune modifying agents:
TNFa inhibitors tend to be first line - adalimumab usually first agent of choice
There are increasingly more biologics becoming available to dermaotlogists for treating psoriasis
ECZEMA
Very common
Prevalence:
Approx 25% (15-44%) < 5 years olds have it incidence of up to 5% in children
Approx 5-10% of adults
Co-association with asthma or allergic rhinitis in up to 50%
Lesions typically occur on flexural surfaces
Is a “barrier defect”- so lets water out of skin and the skin is very dry
Irritants/allergens can easily get into skin causing inflammation
This combination leads to constant itch which makes the inflammation worse and you get a worsening itch scratch cycle
Chronic itching and inflammation can lead to hypo/hyperpigmentation and lichenification (thickened skin with exaggerated skin lines)
It is an itchy condition and patients present with dry skin and an associated red,scaly rash
Often have secondary changes such as scratch marks and excoriations
Can get secondarily infected and can look impetiginised (golden crust) or weepy
With chronic scratching the skin can become thickened with exaggerated skin markins (lichenification) - more noticeable darker skin types
May manifest differently depending on age:
Infants (< 1 year old): often effects face first but can be widespread
School age: flexural pattern, especially elbows and knees
Adults: often localized eczema (such as hands, eyelids, flexures)
Facial eczema infant
Courtesy Dr. McColl
Image courtesy Dr. McColl
Lichenification
Discoid eczema
A common type of eczema in which the patches are roundish (annular/disc shaped). This type can be stubborn to treat and may require stronger topical steroids.
Stubborn discoid eczema
Treatment:
Use of regular emollients extremely important to repair barrier and maintain water in the skin
Topical corticosteroids to decrease inflammation
Oral antihistamines don’t help at all with itch
Sedating antihistamines (eg piriton) should only be used to aid sleep in circumstance that infant is not sleeping
(Topical treatments is obviously a very important thing to be aware about in GP so for more information, click here)
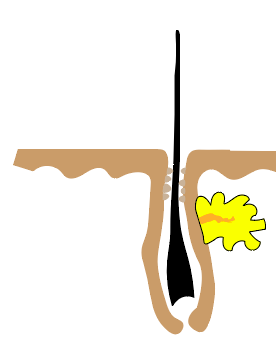
Acne vulgaris
Chronic disorder of pilosebaceous apparatus
Get increased cells building up at infundibulum
Overproduction and build up of sebum
Good haven for colonisation and proliferation of Propionibacterium acnes leading to inflammation
Can enlarge and rupture leading to marked inflammation and scarring
Early commeodne
Hyperkeratosis in infundibulum
Same time get androgen stimulation of sebum secretion
Late commedone
Accumulation of keratin
Inflamm papule/cyst
P acnes proliferation
Sebaceous lobule regression
Nodule/Cyst
Marked inflammation with rupture of apparatus
Can lead to scarring
Characterised in order of increasing severity by:
1/comedones (whiteheads and blackheads)
Commedonal Acne
Closed commedones- whiteheads
2/Papules and pustules
Papulopustular acne
Courtesy Dr. Ian McColl
3/Cysts and nodules
Nodulocystic acne
Courtesy Dr. McColl
4/Scarring- the endpoint we wish to avoid
Scarring from acne
Treating acne:
First line therapy: topical antibiotics (eg tetracyclines), benzyol peroxide or topical retinoids
2nd line: 4-6 months of low dose oral antibiotics such as tetracyclines or erythromcyin.
OCP such as dianette in females (if no contraindication)
Spironolactone occasionally used
3rd line: use of oral retinoids [isotretinoin-only prescribed by specialists]
Isotretinoin (Roaccutane) for acne has many adverse effects but is very effective, SEs include:
Causes marked dryness of skin and mucous membranes (especially lips)
Teratogenic- must exclude pregnancy during treatment as well as at 1 month intervals and should be on 2 forms of contraception
Mood issues. Difficult topic- scattered case reports of suicide with people on roaccutane in the past. Studies difficult to find causal link of roaccutane with mood issues. Risk is low but caution applied if significant personal or family history of depression.
Abnormalities of lipids and LFTs may occur (exclude before treatment and check again at maybe 8 weeks)
Other S.E- paronychia (infection at base of nail), contact lens problems, fragile skin (no waxing during treatment)
Acne fulminans: A rare, systemic disease in which severe and often ulcerating acne is accompanied by fever, arthralgia and occasionally arthritis
Rosacea
Chronic skin condition
Tends to affect cheeks, forehead, chin and nose
Characterised by redness, dilated blood vessels, papules and pustules and often a tendnecy to blush easily
Women more often affected
30-60s
Symptoms/Subtypes:
1/Erythema and telangiectasia of skin
2/Acneform papule and pustule formation are present especially covering cheeks, nose, chin and glabella regions (absent commedones)
3/Rhinophyma (irrregular thickening of skin of nose)
4/Conjunctivitis and blepharitis may be associated (ocular rosacea)
5/Granulomatous rosacea- persistent larger papules and nodules
Different types of rosacea
Facial flushing, papules and pustules
Globalskinatlas
Exacerbations: sunlight, heat, alcohol, consuming spicy food, hot drinks.
To distinguish from acne: absent comedones, distribution of rash (is wider in acne), effect of sunlight, age (acne not as common above 30 but can still occur)
Lichen planus
Autoimmune disease: chronic inflammatory condition.
Immune attack targeted against basal kertinocytes.
All the Ps: Pruritic, purple, polygonal, flat topped papules/plaque often over wrists and ankles. Genitalia also affected often.
Wickham's striae present- fine, white, lacy pattern over the papules
Often get oral involvement- lacy white membrane on buccal surface of cheeks (up to 50%)
Can get nail invovlement (10%)
If affects scalp can get scarring alopecia (called lichen planopilaris)
Like psoriasis shows koebnerisation (eg trauma caues new lesions in that area)
Often idiopathic
Some associations:
Autoimmune liver disease (eg PBC)
Systemic viral disease (eg hep C)
Drugs (Thiazides, ACEi, Antimalarials)
Resolves in 12-18 months.
If mild may give topical steroids to treat symptoms. Could also consider phototherapy (eg uvb)
If more widespread and severe may give course of prednisolone or use another immunosuppressive agent of which there are many.
Courtesy Dr. Ian McColl
Scarring alopecia of lichen planus (lichen planopilaris)- if still active may get erythema around edges of scarring
Erythema nodosum
Acute panniculitis (inflammation of fat layer) that produces painful nodules or plaques usually on the shin.
Commonly seen in:
Infections: eg Streptococcal infections/TB
Inflammatory conditions: Sarcoidosis, IBD
Pregnancy
Medications: Penicillin/OCP/Tetracyclines/sulphonamide/sulphonylureas
Often idiopathic
Treatment:
Treat underlying cause if found
Bed rest
Compression stockings
Anti inflammatories for pain
Tends to go away over a few weeks-months
Pyoderma gangrenosum
Autoinflammatory disorder
Called a neutrophilic dermatosis because lots of neutrophils are seen in the dermis on biopsy
Starts as inflammatory pustules/papules that appear on limbs and trunks
Enlarge rapidly to produce large necrotic ulcers with sloughy base- which undermines a raised purplish prominent rim. Can double size in a week
Biopsy: Intense neutrophilic infiltration in dermis, necrosis of overlying epidermis
Can show pathergy- exaggerated skin injury occuring after minor trauma (eg ulceration occuring at site where bloods were taken)
Associations:
GI- IBD
Rheum- RA, AS
Liver- Chronic hepatitis, PBC, PSC
Haem- Leuk, Lymph, myeloproliferative disorders( PRV, myeloma)
Others- DM, Sarcoid
Treatment:
Medical emergency
High dose Prednisolone to stop rapid growth
Ciclosporin when taper prednisolone
[other regimes may be used sometimes]
Acanthosis nigricans
Get velvety thickening and pigmentation of major flexures (axilla, groin, neck)
Associations-
Stomach cancer [often more florid and late manifestation]
Insulin resistant DM
Obesity
PCOS
Drugs: NODES: nicotinic acid, OCP, dilantin (phenytoin), estrogens, steroids
Erythema multiforme-Steven Johnson syndrome-TENS explained
Old way of thinking: Erythema multiforme- Steven Johnson- TENs were a spectrum of the same disease
This classification can cause alot of confusion
Recent consensus meeting:
E multiforme is one disorder and the Steven johnsons/TEN spectrum is a completely distinct clinical disorder.
1/E multiforme (minor and major): caused by infection or drugs
2/Steven-Johnson/TEN: almost always caused by drugs
E multiforme typical target or raised edematous papules distributed acrally usually. But can be more widespread and involve mucous membranes
SJS/TEN: widespread shallow blisters and erosions and one or more mucous membrane erosions
SJS vs TENS:
Epidermal detachment:
<10% Body surface area Steven-johnson
10-30% SJS/TEN spectrum
>30% TEN
Now into each in more detail:
Erythema multiforme:
Acute self limiting and recurrent condition affecting skin and mucosal surfaces.
Hypersensitivity reaction due to circulating immune complexes (often occurs 7-14 days after initial insult)
Urticaria (hive) like rash with purpura or vesicles in the centre ('target lesion' or 'bull's eye')
Target leisons not always clear cut
Often seen on back of hands, palms and forearms
Erythema multiforme minor: usually acral rash
Erythema multiforme major: involvement of larger body surface area and mucous membranes also
Associated with:
HSV
Mycoplasma pneumonia
Other infection: Hep B, HIV, EBV, Psittacosis, Ricketts, Mumps, Orf
Drugs: Sulfa drugs, Barbiturates, Penicillin
Internal malignancy
Steven Johnson syndrome and TEN
Steven Johnson is a severe reaction in which there is sheet-like skin and mucosal loss (mucous membranes of mouth, eyes, genitalia)
Nearly always caused by medications
100 times more common in association with HIV infection.
Medical emergency
Severe TEN
Toxic epidermal necrolysis:
More severe variant of Steven-Johnson (>30% surface area)
Rash rapidly spreads over body
Begin as large, painful, burning macules- eventually epidermis sheds to reveal a moist dermis layer underneath.
Skin biopsy aids in diagnosis
Management:
Withdraw offending agent, manage them in specialist plastics/burns unit for very careful and skin,oral and eye care
Treat any infections with antibiotics
Use of steroids/other agents is controversial
Causes: [usually occur within first 8 weeks of starting the drug]
Anbibiotics:
-Suflonamides (cotrimoxazole) [often HIV patients on this as PCP prophylaxis]
-Beta-lactams
Anticonvulsants (lamotrigine, carbamazepine, phenytoin, phenobarbitone)
Allopurinol
Anti-inflammatories- NSAIDs
[AAAA]
Henoch-Schonlein-Purpura
Palpable Purpura in dependent areas (buttocks and lower legs)
Form of small vessel vasculitis
4-15 years of age most frequently (can occur at any age)
Male 2:1
Triggers- Streptococcal sore throat, drugs (ACEi,NSAIDs)
Get IgA depostiiton in blood vessel walls
Joint pain
Renal impairment (Severe kidney impairment in 5% of cases)
Abdo pain and minor GI bleeds
IgA elevated in 50%. May be leucocytosis or eosinophilia.
Treatment and recovery:
Prednisolone only for severe GI or renal involvement.
Usually recovery in 4 weeks.
Alopecia- hair loss
Alopecia areata:
Autoimmune condition.
Patchy alopecia:Loss of hair that leaves single or multiple, discrete, often round, areas of shiny baldness on the scalp, beard area or any hair bearing part of body.
Alopecia totalis: all or nearly all of scalp hair gone
Alopecia univeralis: all or nearly all hair from scalp and body gone
Signs:
Disease may be active if see broken hairs at the advancing edge of lesion that look like exclamation marks= these are very short hairs, thicker distally and thinner proximally
Autoimmune associations:
Vitiligo
Thyroid disease
P anaemia
RA
DM
1/3 have positive family history
Many patients experience hair regrowth in 9-12 months, may initially be white hair when comes back.
No scarring occurs with this form of hair loss
Treatment:
Topical steroids, minoxidil, PUVA
[Trichotillomania: self inflicted pulling out of ones hair. Often arises in people with obsessive compulsive disorder. May develop as coping mechanism for stress or anxiety. Exam may reveal irregularly-shaped patches of alopecia.]
[Teloegen effluvuium- generalized hair loss that can occur after an insult ('shock to the system') such as an infection, general anaesthetic. Can occur 2 months after initial insult.]
Causes of hair loss with scarring:
Discoid lupus erythematous
Lichen planus
Scleroderma
Radiodermatitis
Hair follicle destroyed in all above. Regrowth never occurs.
Blistering conditions
1/ Dermatitis Herpetiformis
Extremely itchy condition associated with gluten-sensitive enteropathy (which may be asymptomatic)
Most common in 3rd or 4th decade
Get erythematous rash on extensor surfaces (elbow, buttocks, shoulder, scalp)
Small vesicles present
Mucous membranes may be affected.
Skin biopsy shows IgA deposits in unaffected skin
Treatment- dapsone (for itch-works almost immediately) and gluten free diet.
Global skin atlas
Global skin atlas
Less then 10% have symptoms of gluten senisitive enteropathy
Greater then 90% have abnormalities on endoscopy with 2/3 show villous atrophy on biopsy
Bullous Pemphigoid
Disease of the elderly (over 60)
Presnts with TENSE blisters with surrounding urticarial rash
Autoimmune blistering disorder characterised by presence of IgG autoantiboides to components ofthe basement membrane.
Split is deep occuring between epidermis and dermis so that blisters are tense and do not spontaneously rupture
Mouth involved in only 10%
Treatment: high dose oral steroids and taper down to dose that keeps blisters at bay.
Pemphigus vulgaris
Flaccid blisters, often present as erosions
Large areas of body can be affected and mortality without treatment is high
Mucosal involvement with ulceration (presenting sign in up to 50%)
Get soreness from blisters as they rapidly denude(appearance often one of weeping erosions)
Blisters can be extended with gentle pressure (Nikolsky's sign)
Due to deposition of IgG in epidermis, desposition higher then in bullous pemphigoid
Skin biopsy- intraepidermal split above basal layer
Treatment- high dose steroids and azathioprine (as long term maintenance)
May have increased risk of skin malignancy
Porphyria cutanea tarda
Clinical effects due to increased porphyrins in blood stream. [porhyrins are part of metabolic pathway to produce haem]
Can be inherited
Usually acquired due to liver damage: get acquired decreased activity of liver enzyme uroporphyrinogen decarboxylase which blocks the pathway leading to increased porphyrins in bloodstream
[Predisposing factors- Alcohol, smoking, oestrogens, Hep C, Haemochromatosis]
Porphyrins enter into the skin and are activated by UV light causing damage locally and giving the clinical effects
Classic example is person that is away on holiday and drinking alot. The liver damage releases porphyrins into the blood and the skin. The UV light activates them causing the damage
Presents with bullous eruptions (blisters) on exposure to sunlight.
These heal with scarring and milia (small cysts)
Also get hypertrichosis (excess hair)
Courtesy Dr. McColl
Diagnosis: increased levels of plasma AND urinary porphyrins!!!
Treatment:
Sun protection, cut down alcohol
Repeated venesection
Chloroquine
Diagnosis depends on increased levels of plasma and urinary uroporphyrins
[In clinic if examine urine with Wood's lamp- urine shows pink fluorescence (shows urine porphyrins)]
[If have similar clinical features but porphyrin levels are normal it could be pseudoporphyria which is often a reaction to medications eg NSAIDs]
Necrobiosis lipoidica
Unusual complication of DM (may also occur in non diabetics)
Due to small vessel damage leading to partial necrosis of dermal collagen
Skin appears thinned
More commonly seen in young/middle aged females
Skin over shins most commonly affected (often presents as erythemaous plaques that gradually develop a yellow-brown waxy discolouration with visible telangiectasia)
Treatment- support bandaging. Low dose aspirin helps healing.
Necrobiosis lipoidica
Dermatomyositis
When develops over 40 years- 1/3 of patients have a carcinoma
More common in females.
Rash affects face and often extensor bony prominences of shoulder and limbs and back of hands.
Puffy, red, upper outer eyelids often seen (heliotrope rash)
Rash can be seen on knuckles and dorsal fingers (Gottron's papules)
Gross dilatation of the posterior nail fold capillaries.
Generalized photosensitive rash
Weakness of the major proximal muscle groups is also commonly seen.
Rarely involuntary muscles affected (swallowing or breathing difficulties)
Calcification in deep muscle plains occurs in childhood
Diagnosis:
Raised CPK
Muscle biopsy confirms
Most ANA positive
Presence of anti-Jo1 associated with pulmonary involvement.
Heliotrope rash
Photosensitive distribution
Gottron's papules- erythema which is localized over the knuckles
Also can get dilatation of vessels in proximal nail fold
Lupus
Chronic discoid lupus erythematous:
Most patients with discoid lupus just have skin involvement (but 5-25% can develop SLE)
Affects sun-exposed areas
Affects face, neck, scalp and hands (female:male 2:1)
Well-demarcated plaques of scaling erythema that progress to atrophy
Plaques heal with scarring, pigment change (tend to look darker on caucasian skin/pale on black skin) and telangiectasia
Scalp lesions destroy hair bulbs leading to scarring alopecia
Diagnose often made by skin biopsy
Small proportion have circulating ANA which may indicate risk of progression to systemic lupus.
Treatment- topical sun-block and steroid creams
Systemic therapy- hydroxychloroquine (aka plaquenil)
Discoid lupus face
Scarring alopecia in discoid lupus
Subacute Lupus:
Precipitated by sun exposure
Can look like psoriatic type papulosquamous rash or get annular (circular) plaques that are clear centrally. No scarring.
Medium assocaition with SLE
Anti-Ro positivity high in this population
Can be due to drugs (anti seizure meds, anti-TNF, PPIs)
Acute cutaneous lupus:
Highest association with a SLE
Classic presentation is the malar eruption or 'butterfly rash'
Other variants of acute lupus: photosensitivity, bullous lupus, chelitis and mouth ulcers, papular rash on arms which can form large plaques
Systemic sclerosis
Features include-
Firm skin which may be discoloured sometimes with 'salt and pepper discolouration'
Microstomia
Facial telangiectasia
Beaking of the nose.
Raynaud's is seen in 90-95% with systemic scloerosis (colour change: white to blue to red
Male:female SS 1:3
Usually divided into 2 subsets: limited and diffuse.
Limited: Skin affected below elbows and knees (can involve the face)- associated with features of CREST sydnrome. Anti-centromere antibody strongly associated with limited and CREST.
CREST syndrome (calcinosis, raynaud's, esophageal dysmotility, sclerodactyly, telangiectasia)
Diffuse: Skin affected can be above elbows and knees on the body. This subtype more likely to have kidney, heart and joint problems.
Scl-70 is unique to systemic sclerosis and is more likely to be associated with severe disease affecting the lungs. Commoner in diffuse subtype.
ANA positive in majority of subtypes of systemic sclerosis.
Lung involvement can occur in systemic scleorsis:
1/Pulmonary vascular disorder evolving over time into pulmonary hypertension
2/Interstitial lung disease.
Transfer factor is reduced with pulmonary fibrosis - this is the earliest sign of fibrosis in systemic sclerosis;
Sclerodactyly (tapering of fingers)
Courtesy Dr. McColl
Courtesy Dr.McColl
Lupus Pernio:
Due to sarcoid disease. Can get diffuse bluish plaque on nose and on closer insepction small red papules in lesion , can also get on ear lobes.
[will aim to get picture of this]
Pretibial myxoedema
Is a rare complication of Grave's disease.
Get raised indurated pinkish patches.
Can occur anywhere but typically occurs on the shins and dorsum of the feet.
High titre of TSH receptor antibodies would be expected
Waxy papules seen in pretibial myxoedema. If knick one of them might see release of a mucinous fluid.
Globalskinatlas
Bacterial infections
Impetigo:
Impetigo is a common bacterial skin infection.
Usually due to Staph aureus but can be due to beta haemolytic strep also (eg strep pyogenes)
Can get pustules and the classic honeycomb coloured crusted erosions.
One subtype is bullous impetigo in which you can get blisters which occurs due to staph exfoliative toxins
Local- topical antibiotics (eg mupirocin)
Widespread- oral flucloxacillin
Non bullous impetigo
Globalskinatlas
Erysipelas:
More superficial form of cellulitis
Unlike cellulitis almost all cases are casused by Group A beta haemolytic strep (strep pyogenes)
Get distinctive warm, red, tender skin lesion with induration and sharply defined, raised, rapidly advancing border
Vesicles or bullae may develop.
legs and face are comonly affected
Raised WCC, blood cultures positive in 5% of patients
Treatment is with IV antibiotics such as benzylpenicillin and erythromycin.
Ddx:
DVT, necrotising fasciitis, contact dermatitis
The infection can cause damage to the surrounding lymphatics leaving the patient prone to lymphoedmea and recurrence of hte infection
Usually erysipleas is unilateral but in this unusual case it was bilateral
Courtesy Dr. McColl
Blistering secondary to erysipelas
Fungal infections
Dermatophytes:
Diagnosis made by microscopy of scrapings taken from lesion.
Clinical: Get erythematous plaques with scaling border and area of healing in the centre
Dermatophytes named tinea. Then named depending on the location of the infection irregardless of the type of microorganism.
Tinea Coroporis: body
Tinea Pedis: feet
Tinea cruris- more common in men and also during hot and humid seasons. It may extend to the inner thighs and backwards to the perineum and anus. Most often the infection spreads from the toe webs to the groin.
Tinea manum: Can get a dry and scaly form which commonly affects only one hand. The feet should be examinesd as they are often infected.
Tinea pedis: Commonest fungal infection. Primary lesions consist of maceration, scaling, occasional vesicles and fissures between and underneath the toes. Any or all of the toe webs may be affected although the most affected web space is the fourth.
Onychomycosis: Tinea affecting nails represents about 30% of all superficial fungal infections. Nails are usually discoloured soft, brittle and may loosen away from the nail bed . Commonest form starts distally in the nail plate.
Tinea incognito:
The name given to tinea when appearance has been altered by inappropriate treatment (usually topical steroid cream)
Original infection slowly extends
Often doctors thinks its a dermatitis instead of fungal infection
The steroid cream dampens down inflammation but when cream is stopped for a few days the rash gets worse and has altered appearance
Courtesy dr. McColl
Tinea capitis (infection of scalp) due to T. Tonsurans, M. Canis, T. Rubrum or T. Verrucosum
M canis is zoophilic (derived from animals)
Tinea capitis
Globalskinconsult
Boggy swelling (kerion) seen in severe fungal infection scalp
Favus:
A type of tinea capitis. Is rare in the UK and USA but get in middle east, south east europe, mediterranean and africa. Cup shaped crusts called scutulae form around loose hairs. Scarring alopecia is common.
Due to Trichophyton schoenleinii
When the lesions fall off the portion of scalp affected is usually hairless.
Tinea diagnosis: Microscopy of scrapings in potassium hydroxide
Tinea management:
Topical preparation such as miconazole (daktarin) or ketoconazole
More severe- oral antifngals (eg itraconazole)
[prolonged treatment for up to 4-6 weeks is usually required for body/scalp lesion, up to 6 months for nail infections]
Candida:
A group of yeasts
Particularly affects moist areas such as flexural areas like the groin and under the breast
Commonly seen under occluded surfaces so often in nappy rash
Often see satellite lesions extending beyond the main rash
More common in immunosuppressed patients (eg DM/HIV/Steroids)
Can get oral candida and vaginal candida infection
Satellite lesions of candida
Herpes family:
Herpes Simplex Virus:
Localized vesicles and blistering.
Oral involvement more frequently due to HSV 1
Genital ulcers: herpetic ulcers are the commonest cause of genital ulcerations in the developed world. 80% are caused by HSV 2 and 20% by HSV 1. Primary lesions are painful and associated with enlarged lymph nodes.
Treat with antiviral (eg aciclovir, valciclovir)
Eczema herpeticum- patients with atopic eczema are prone to infections with HSV which become disseminated throughout the eczematous areas (aka Kaposi's varicelliform eruption)
Patient can be unwell and is medical emergency
If affects eye can cause blindness if not treated appropriately
Treatment with acyclovir required
Suspect when get severe flare of eczema with punched out lesions.
Chicken pox (varicella): distributed centripetally with trunk affected more than extremities. Individual lesions are in various stages of development (macules, papules, vesicles, crusted and healed lesions).
Classical lesion that is often cited is the dew drop on a rose petal appearance.
'Dew drop on rose petal' lesions
Chickenpox in adults:
More serious then in children.
Varicella pneumonia occurs in up to 20% of adults with chickenpox occuring 3-5 days into the course of the illness.
Symptoms include
Tachypnoea, cough, dyspnoea, fever.
Cyanosis, pleuritic chest pain and haemoptysis are common
Treat with aciclovir
Zoster (shingles): more common in elderly and immunosupressed. It is caused by activation of dormant virus which has been living in dorsal root ganglia nerve cells in the spine after previous exposure to chicken pox. When reactivated it migrates down the sensory nerves to cause herpes zoster lesions. Pain preceding the characteristic vesicular lesions is typical.
Special cases Zoster infection:
Post herpetic neuralgia- can persist for years. Treatment is challenging and patients may require antidepressants, carbamazepine or ablation of the affected ganglion.
Ramsay Hunt- get reactivation of the zoster virus in the geniculate ganglion (collection of sensory neurons of the facial nerve) resulting in pain and vesicles in the ear, ipsilateral facial palsy and sometimes impairment of taste on the same side.
If the opthalmic branch of the trigmeninal nerve is affected - may cause corneal ulcers and blindness.
Herpes simplex infection of the eye in general often affects the cornea (keratitis) and can lead to corneal ulcers ('dendritic'-branching ulcers). Recurrences are common and may result in blindness.
Herpetic whitlow: was commonly seen in dentists, dental hygienists and other health workers before universal use of gloves. Now more common in children. Get pain and vesicles/blistering in pulp of finger. Can get tenderness, erythema and deep seated blisters in nail fold.
Molluscum Contagiosum:
Umbillicated, pearly papules 2-5mm in diameter
Often seen in childhood
Caused by a DNA pox virus called molluscum contagiosum virus (MCV)
Commonly occur on face, especially near the eyelids; also occur on genitals and trunk
Treat with cryotherapy, liquid nitrogen or curretage.
Can be seen in patients with advanced HIV/AIDs
Genital ulcers
Syphillis:
Primary syphillis:
Chancre: Small, firm and painless ulcer
Can get lympadenopahty close to ulcer.
Secondary syphillis:
Develops 4-12 weeks after primary infection.
Characterised by :
Macular or papular rash which is symmetrical on the trunk and limbs as well as the palms and soles
Rash is pale pink and non itching
Confluent plaques (conylomata lata) may form in moist flexures (eg groin, around buttocks)
Small grey or white erosions may be seen on buccal mucosa
Patients may get muscle and joint pains, headaches and fevers
Generalized lymphadenopahty is common.
Macular or papular rash
Palms and soles affected
Image courtesy: Dr. Ian McColl
Chancroid:
Caused by H ducreyi and is commonest cause of genital uclers in Africa (4-7 day incubation period)
Erythemaous papule breaks down into a painful ulcer and several ucler merge to form giant lesions
See ulcers on prepuce and freunulum and vaginal entrance and perineum i women
Get inguinal lymphadenopathy which is usually unilateral and can suppurate
Diagnosis: isolating organism from swabs and culturing on chocolate based media
Treatment- co-trimoxazole or tetracycline.
Image courtesy: Dr. Ian McCOll
Tumours
SCC:
SCC spectrum:
Actinic (solar) keratosis-----SCCis (aka Bowen's disease)-----SCC
Actinic keratosis (scaly erythematous areas)- dysp
SCC in situ (aka Bowen's disease)- thicker plaques, often seen on legs in elderly patients
Image courtesy Dr. Ian McColl
SCC (tips that is invasive: tenderness and induration under skin)
Squamous cell carcinoma: malignancy of keratinocytes
Seldom seen in people aged under 45.
Usually occurs in sun exposed areas such as the face and lower lips. It is the second most common type of non-melanoma skin cancer (after BCC)
On exam is often tender and often indurated
Mets- spreads to distant sites by lymphatic channels
Risk of mets- depends on size and location. (ears and lips high risk of mets)
Diagnosis and treatment:
Biopsy for diagnosis
Radical surgery and sometimes radiotherapy. (95% cure rate if prompt and complete excision carried out)
40% risk of developing additional SCC in next 2 years.
Prognosis:
5 year survival 73%
Keratocanthoma-
Low grade malignancy that resembles squamous cell carcinoma pathologically. It is seen mostly on sun exposed sites.
Develops from hair follicle, more common in males.
It is usually solitary but may be multiple. It presents as a fleshy, elevated and nodular lesion with a central hyperkeratotic core.
Most significant feature is its rapid growth.
Short history and rapid increase in size suggest kerathoacanthoma rather than squamous cell carcinoma.
Don't spread elsewhere.
Basal cell carcinomas:
Commonest cutaneous neoplasm in humans (85% are on head and neck)
Major RF BCC is sun exposure
Nodular basal cell carcinoma:
Commonest facial BCC
Prominent telangiectasic vessels on surface of lesion
Border of lesion is translucent, looks pearly white and is slightly raised
Large nodular BCC with ulceration centrally
Superficial BCC occur more frequently on trunk and extemities and present with scaling, irregular plaque. Again have pearly-white raised border.
Morphoeic BCC (aka sclerosing BCC)
Waxy, scar-liiek plaque with indistinct borders
Get wide and deep subclinical extension so need to be very careful with these
Rare compared to other BCCs
Courtesy Dr. Ian McColl
Treatment and prognosis:
Excision surgery for large and deep tumours (nodular, morephoeic)
For superficial BCCs can consider cryotherapy, certain topical agents and photodynamic therapy
Cure in more than 90%
Moreaphorm BCCshave highest recurrence
Melanoma: malignancy of melanocytes
ABCDE criteria for diagnoisis
Asymmetry
Border irregularity
Colour variability
Diameter >5mm
Evolving lesion with changes over time
(also look for bleeding, itching, satellite lesions)
Excision biopsy is key for diagnosis and determining prognosis with Breslow's thickness
Superficial spreading melanoma (commonest)
Nodular melanoma can be amelanotic
Acral lentiginous melanoma:
Normally seen on sole of foot and occasionally or palm of hand
Seen often in darkly skinned races
Poor prognosis
Subungual melanoma
Subungual melanoma with hutchinson's nail sign (pigmented proximal nail fold)
-pointer to malignant melanoma
Lentigo maligna
Represents increased number of atypical looking melanocytes at dermo-epidermal junction
Is a type of malignant melanoma in situ
Occurs on facial or sun-exposed skin of patients in their 60s or older
Often very slow growing over years-decades
If invades the dermis is then a lentigo maligna melanoma and behaves like a melanoma (suspect if get thick, darker or get discrete nodules)
Lentigo malgina
Nodular lesion representing lentigo maligna becoming a lentigo maligna melanoma
Other tumours
Mycosis fungoides (cutaneous T cell lymphoma)
Atypical lymphocytes seen in epidermis and dermis
Usually has low grade clinical course and can remain in one stage (patch-plaque-tumour) for a number of years
Initially presents as a pruritic eczematous rash (pre malignant). Can get an appearance of "cigarette paper" atrophy on the surface. Lesion slowly progresses to thick plaque.
As more lymphocytes infiltrate it progresses from a patch to a plaque to a thick tumour
As malignancy develops nodular lesions appear and proceed to become necrotic.
Patch stage MF
Globalskinatlas
Plaque MF
Tumour MF
Kaposi's sarcoma:
Associated with HHV 8
Is a reactive hyperplasia of the vascular endothelial cells. Not really a neoplastic lesion
Lesions are blue-red, firm, warty and neither painful nor itchy.
Nowadays usually seen in young HIV positive men (lesions found here on tip on nose,neck and buccal mucosa)
Prior to AIDs epidemic- a rare tumour of elderly men affecting the legs usually and associated with lymphoedema
Likely viral cause
Pityriasis rosea
First clinical lesion in pityriasis rosea- “herald patch” which is an isolated erythematous patch appearing on the trunk surrounded by ring of scaling skin
A number of oval macules appear on the upper arms, remainder of trunk and upper thighs about 2-4 days later. Tend to spread out along rib cage in a 'fir tree' type pattern
Involvement of hands, feet or scalp is rare
Severe itch uncommon
Usually remits within 4-8 weeks.
Occurs more in Spring and Autumn
Treatment:
No specific treatment
Systemic antihistamines, moisturisers may help with itch.
Topical steroids don't shorten duration of disease.
Herald patch
Annular to oval shaped lesions in a 'fir tree' pattern
Scabies
Due to parasitic mite Sarcoptes scabiei
Itchy excoriated papules on finger webs, elbows, ankles, axilla and genitalia
Rarely causes blistering
Burrows of the scabies mite are seen and patchy excoriated fissured eczema occurs
Adult males develop itchy penile nodules. Infants get nodules on palms or soles
Treatment: Permethrin cream (lyclear) to whole body at day 0 and day 7.
Scabies
Courtesy of Dr. McColl
Scabies burrows
Erythroderma
Any inflammatory skin disorder covering in excess of 90% of the body surface leading to skin failure.
In adults most common is eczema followed by psoriasis, leukaemia/lymphoma, drugs and a condition called pityriasis rubra pilaris
Sequelae include high output cardiac failure, hypothermia, loss of fluid and albumin and increased susceptibility to infection.
Erythroderma- in this case due to psoriasis
Behcet's Disease
Classic triad- recurrent oral ulcers, recurrent genital ulcers, iritis.
Recurrent oral ulceration. Can effect eyes causing blindness. Also can get genital ulceration. Diagnosed aided by a positive skin pathergy test (development of pustules at venepuncture sites)
Other features- fever, abdo pain, diarrhoea, episcleritis, polyarteritis, arterial and venous thrombosis, pericarditis.
HLA B5 associated with ocular disease; HLA B12 with reurrent oral ulcers.
Treatment is with steroids or colchicine.
Reactive arthritis: with other classic features is called Reiter's syndrome
Autoimmune reaction to an infectious agent [bacteria- genitals (chlamdiya), bowel (campylobacter, shigella, salmonella)]
Classic triad of:
1/Non-suppurative polyarthritis
2/Inflammatory eye disease (Conjunctivitis early and may be followed by iritis)
3/Urethritis
[can't see, can't pee, can't climb a tree (arthritis usually affects lower limbs)]
Skin lesions often occur on the feet with pustules and hyperkeratosis (keratoderma blennorhagicum) May also get erosive lesions affecting penis (circinate balanitis) or mouth
Rare complications- heart block, aortic incompetence, pericarditis.
Keratoderma blennorhagicum
Images courtesy Dr. McColl
Pigmentary disorders
Melasma:
Hormonally stimulated increase in melanin pigment that mainly appears on face (affects both pregnant women and those taking the OCP)
Get hyperpigmentation which is augmented by sunlight.
Takes many months to resolve after delivery
MSH levels are normal
Affects women with darker skin tones
Morphoea (aka localised scleroderma)
Firm, white or violaceious patch of thickened skin on any body site (usually thighs, trunk and upper arms)
Affects kids and young adults
Developing lesions have well demarcated red or violet peripheral edge
As activity burns out- the edge assume the same colour as the central lesion and lesion itself becomes very firm with atrophic glazed surface appearance
A linear variant of morphoea may be seen on scalp and face of kids (en coup de sabre)
En coup de sabre
Vitiligo:
Autoimmune condition
Acquired areas of skin depigmentation due to loss of melanocyte function
Associated with type 1 DM, coeliac disease, autoimmune thyroid and Addison's
Biopsy- epidermal melanocytes lost from basal layer of epidermis
Treatment generally unsatisfactory
Condition also occurs in darker skinned races
Albinism:
Group of inherited abnormalities of melanin synthesis charcterised by congenital reduction/absence of melanin pigment in association with specific developmental changes in the optic system resulting from hypopigmentation.
At much increased incrased risk of skin cancers due to lack of protective pigmen
Oculocutaneous albinism involves 2 regions of body:
Skin and hair
Optic system including eye and optic nerves.
Ocular albinism- just optic system affected
Pityriasis versicolor
Caused by yeast malassezia furfur (normal commensal but causes this reaction in some people)
White untanned skin: pale brown/pink macules which are often hardly visible
Tanned skin: appears pale, white and slightly scaly (yeast affects tanning)
Diganosis:
Wood’s light: yellow green fluorescence
Microscopy: hyphae and yeast cells (spaghetti and meatballs)
Looks pink on white skin
Can look white/pale on tanned skin
Spaghetti (hyphae) and meatballs (yeast)
Treatment:
Topical antifungals (clotrimazole, terbinafine)
Systemic antifungals rarely required
Condition can recur.
Seborrhoeic dermatitis
Caused by a yeast infection (malassezia furfur)
Is very common in immunosupressed patients and neuro patients (parkinson’s)
Treat with topical antifungal (eg miconazole)
Genodermatoses
Tuberous sclerosis
AD with variable expression
Epilepsy in infancy or childhood
Mental reatardation often seen
Angiofibromas
Elevated hypopigmented macules (ash leaf pathces) often seen
Periungal fibromas arise as pink projections from nail folds
Shagreen patch is angiofibromatous raised plaque usually on back
Fundoscopy may reveal white streaks along fundal vessels
Small pink/red spots across cheek and nose in butterfly distribution
Globalskinatlas
Periungual fibromas- not the best image. Often pink small nodules around nail
Ash leaf macule
Shagreen patch- area thick leathery skin
Neurofibromatosis:
Type 1: mixture of skin features: cafe au lait spots (>6), axillary freckling, cutaneous neurofibromas, lisch nodules (multiple brown deposits in the iris of the eye), optic nerve gliomas.
Develop over years but pace may increase with puberty and pregnancy.
Many other features:
HTN
Learning difficulties/behavior problems
Neurofibromas
Cafe au lait spots
Axillary freckling
Type 2:
Not as many skin features
More CNS tumours (acoustic neurofibromas common)
Juvenile cataracts