The first video covers from the introduction to severity assessment - the times to the relevant sections are noted in the headings
Introduction - epidemiology (01:30), causes (02.25), exacerbating factors (03.45), pathogenesis (06.15)
Subtypes: (07.44)
Chronic plaque psoriasis (07.50)
Guttate psoriasis (10.15)
Pustular psoriasis (11.15)
Palmoplantar pustulosis (16.20)
Acrodermatitis of hallopeau (17.35)
Erythrodermic psoriasis (18.15)
Histopathology (19.10)
Psoriasis associations (20:15)
Nail psoriasis (22.20)
Psoriatic arthritis (24:20)
Severity assessment (26:00)
INTRODUCTION
Psoriasis is a chronic inflammatory skin condition and one of the commonest conditions we see in dermatology
Epidemiology:
Affects 2-3% population in Europe
Affects men and women equally but men more likely to have severe disease
Tends to persist lifelong, fluctuating in extent and severity
About 1/3 of patients with psoriasis have family members with psoriasis
Age at onset:
Bimodal
Early onset < 30 years (Peak 16-22)
75%
HLA-Cw6 association
More likely to have familly history
More likely to be severe, unstable disease
Late onset > 40 years (Peak 55-60)
Sporadic and not HLA associated
What casuses psoriasis:
Genetics, environmental factors and the immune system all play a role in the pathogenesis of psoraisis
Genetics:
Studies have reported 72% concordance in monozygotic twins and 23% in dizygotic twins
More recently genome wide association analysis has mapped at least 80 loci that can be associated with psoriasis
The major psoraisis susceptibility locus is termed PSORS1 and lies within the major histocompatibility complex (MHC) on chromosome 6
Within this locus, HLA-C*06:02 is the genetic variant that makes the largest contribution to psoriasis susceptibility
Inheritance of one allele of HLA-C*6:02: increases risk of psoriasis 4-5 times
Environmental factors:
Infection:
Streptococcal infection can cause a flare of psoriasis (eg guttate psoriasis)
Interestingly get a similar T cell repertoire in infected tonsils as is found in the skin in psoriasis
Medications:
Steroids (it is important to be aware of the risk of a flare or development of pustular psoriasis on withdrawal of steroids)
Lithium, beta blockers, systemic anti-malarials, intereron-alpha
TNFa inhibitors: can get paradoxical psoriasis affecting palmoplantar areas and scalp (this is a class effect so if get with one TNFa inhibitor likely to get with another)
Smoking:
The Rate of smoking is increased in psoriasis patients compared to normal population
Palmoplantar pustulosis is almost exclusively seen in smokers but it is still unclear if smoking cessation helps improve it once it has developed
Psychological distress:
Up to 80% report worsening of psoriasis in relation to psychological stress
Endocrine factors:
Pregnancy (although psoriasis often improves during pregnancy thankfully)
Hypocalcaemia
Physical trauma:
Koebnerisation (appearance of skin lesions of a pre-existing dermatosis on areas of cutaneous injury)
(other causes of koebner phenomenon - lichen planus, vitiligo, molluscum contagiosum, bullous pemphigoid)
Role of immune system:
Psoriasis is a T-cell mediated disorder primarily driven by pathogenic T cells
It involves prominent involvement of helper T-cells and their secreted cytokines
Increased levels of T helper 1(Th1) and Th helper 17 (Th17) subsets and each subset secretes their own ‘signature’ cytokines
The cytokines TNFa, IL 12, IL 23 and IL 17 all contribute to the disease and as such are the targets of the different biologic treatments
The T cells interact with dendritic cells, keratinocytes and neutrophils under the influence of various cytokines and this process leads to keratinocyte proliferation, neutrophil chemotaxis and angiogenesis which leads to a psoriatic plaque
Of note, Keratinocytes tend to move from basal layer to upper layer in 3-5 days (compared to normal of 28 days)
Click here to skip to discussion about biologics and cytokines pathway which is discussed in greater detail
CHRONIC PLAQUE PSORIASIS
Symmetric distribution of demarcated plaques
‘Salmon pink in colour with silvery scale’
Common sites:
Scalp
Extensors elbows and knees
Sacrum
Hands and feet
Other areas to look for as a clue it may be psoriasis: behind the ears, the nape of the neck, the umbilicus
Ranges from mild to very extensive
Courtesy Dr. McColl
Globalskinatlas
Scalp psoriasis: can be difficult to treat and can have significant affect on quality of life
Scalp psoriasis
Courtesy Dr. McColl
Flexural psoriasis:
The moist occlusive surfaces prevent build up of scale - appears red, macerated and shiny
Often get overgrowth of candida (see satellite lesions) so often use combination medication such as trimovate (moderate steroid, antibacterial, antifungal) or lotriderm (potent steroid, antifungal - for very short period as have much higher risk of steroid side effect in these areas)
Flexural psoriasis
Globalskinatlas
Genital psoriasis:
Is very important to ask about as it can cause issues with sexual function and can be very difficult to treat
Patients often reluctant to disclose it is an issue
GUTTATE PSORIASIS
Widespread small plaques
Gutta is latin for ‘rain drop’
Commonly seen in children following a streptococcal infection (look for elevated ASOT)
Generally is self resolving over 3 months
40% of patients with guttate psoriasis will go on to form chronic plaque psoriasis
Guttate psoriasis
PUSTULAR PSORIASIS
Can be generalised or localised
Generalised:
Acute generalised (pustular psoriasis of von zumbusch)
Subacute annular and circinate pustular psoriasis (like plaque psoriasis but with pustules within the plaques- patients usually are well)
Acute generalised pustular psoriasis of pregnancy
Localised:
Palmoplantar pustulosis
Acrodermatitis of hallopeau
Acute generalised pustular psoriasis
2 main groups:
Arising in chronic plaque psoraisis patients with triggering factors:
Pregnancy
Sudden withdrawal of steroids
Other medications (beta blockers, aspirin, anti-inflammatories)
Infection
Hypocalcaemia
2. Generalised pustular psoriasis arising de novo:
May be the only manifestation of psoraisis
Recent research suggests that generalised pustular psoriasis and palmoplantar pustulosis are actually distinct from classical psoriasis with a different pattern of immune activation:
Generalised pustular psoriasis alone can be associated with IL 36 receptor antagonist mutations
Generalised pustular psoraisis in patients with preceding chronic plaque psoriasis can be associated with CARD14 mutations
Clinical presentation of acute generalised pustular psoriasis:
Often precipitated by burning sensation, dryness and tender skin
Develop ‘lakes’ and plaques of pustules
Can lead to erythroderma
As pustules dry you get exfoliation
Nails often involved
It is a dermatological emergency - patient scan be unwell with systemic inflammatory response syndrome (SIRS), can get:
Electrolyte abnormalities, dehydration and tachycardia
Fevers
Elevated inflammatory markers
Management of acute generalised pustular psoriasis:
Admit patient
Screen for infection!!!
(Can sometimes be difficult to tell if patient is septic or if it is simply a severe SIRS response)
Regular emollients (emollin spray is a good option)
Some don’t use topical steroids in case it exacerbates a flare when stop them but some cases a moderate topical steroid may be used
Non-adhesive dressings
Analgesia
Hydration
Monitor bloods
In some cases could consider ciclosporin but it can be hard to tell sometimes if there is an underlying infection driving the pustular psoraisis so can be a tough judgement call
PALMOPLANTAR PUSTULOSIS
Pustuolosis of palms and soles
Almost exclusively seen in smokers
Sterile pustules remain localized to palmoplantar surfaces
Pustules are very superficial and dry out leaving brown adherent scale which peels off
Patients often report a sensation of it feeling like walking on glass
Disease runs a chronic course
Often don’t have any psoriasis elsewhere
Globalskinatlas
ACRODERMATITIS OF HALLOPEAU
Sterile pustules starting at tips of fingers/toes and that spread proximally
Nail can become severely dystrophic and can lose the nail
Terminal digit may atrophy (acral osteolysis)
Can be very difficult to treat
Options: ciclosporin (but generally don’t want to be on for long time), acitretin, some reports showing efficacy with apremilast
ERYTHRODERMIC PSORIASIS
> 80% Body surface area affected
Problems with temperature reguation, fluid loss
HISTOPATHOLOGY
(superficially to deep)
Neutrophils in stratum corneum
Parakeratosis
Loss of granular layer
Psoriasiform hyperplasia of epidermis
Thinning of suprapapillary plates
Capillary dilatation and oedema in dermal papillae
Superficial perivascular lymphocytic infiltrate
Neutrophil collections:
Munro microabscesses: collection of neutrophils within the stratum corneum
Spongiform pustule of Kogoj: subcorneal collection of neutrophils
PSORIASIS ASSOCIATIONS
Think of psoriasis as a systemic inflammatory disease with multiple associations so need to consider these during consultations
Psoriatic arthritis
Nail psoriasis
Metabolic syndrome
Hypertenison
Dyslipiadaemia
Insulin resistant DM
Obesity
Higher CVD risk
Psychosocial:
Reactive depression
UK GP database: psoriasis patients more likely to have diagnosis of depression (HR 1.39 CI 1.37-1.41)
Approx 20% patients require treatment with antidepressants
Higher rates of suicidal ideation
Alcohol:
Excess alcohol/alcohol misuse reported in 1/3 of patients with moderate-severe psoriasis
Associated with more severe disease
Important to screen for
Inflammatory bowel disease
Ocular inflammation (iritis, uveitis, episcleritis)
NAIL PSORIASIS
Present in apporx 45% of patients with psoriasis
80% of patients with psoriatic arthritis have nail psoriasis
If nail matrix affected can get pitting (eg if focal part matrix affected), ridging and nail dysrophy (eg if all matrix affected)
If nail bed affected get nail lifted off the bed - oil drops, subungual hyperkeratosis, distal onycholysis
Can see splinter haemorrhages also
Topical preparations don’t penetrate nail bed or nail matrix making treatment very difficult
PSORIATIC ARTHRITIS
15-30% of patients with cutaneous psoriasis
Can occur prior to skin involvement but majority of the time occurs after skin invovlement
Presentations:
DRAMA
DIP joint predominant disease
Rheumatoid arthirits like presentation
Asymmetric oligoarthritis
arthritis Mutilans (grossly deformed hands and/or feet - seen less frequently now due to better treatments)
Ankylosing spondylitis like arhritis
For more info on psoriatic arthritis see end of notes or click here
SEVERITY ASSESSMENT
Different severity scores can be used to measure how clinically severe the psoriasis is, how it affects a patient’s quality of life and to screen for psoriatic arthritis
These scores are sometimes used when assessing whether a patient is a candidate for a systemic agent
PASI -
Measures the severity and extent of psoraisis
Based on body surface area affected and the degree of erythema, induration and scaling in different parts of the body
You can download a pasi calculator app on your phone or simply look it up online - here is a link to the calculator I use:
Psoriasis Area Severity Index (PASI) Calculator (corti.li)
DLQI -
A questionnaire for a variety of skin diseases (not specific to psoriasis)
Measures the impact that a skin disease has a patient’s quality of life
Scored out of 30 and asks how the skin disease has impacted the patient over the last 7 days
Again a simple google will bring this questionnaire up (although it is usually quite easy to find one in a dermatology clinic)
PEST score -
A screening tool for psoriatic arthritis
Patient with psoriasis who do not have a diagnosis of PsA should ideally complete an annual PEST score
A score of 3 or more indicates consideration of rheumatology referral
The questionnaire asks patients to tick the joints that are affected on an image and asks the following questions:
Have you ever had a swollen joint (or joints)?
Has a doctor ever told you that you have arthritis?
Do your finger nails or toenails have holes or pits?
Have you had pain in your heel?
Have you a finger or toe that was completely swollen and painful for no apparent reason?
TOPICAL TREATMENT
Emollients:
Encourage regular use of emollients - greasy ointment preparations tend to be better
(see eczema section or click link here for further info on emollients)
Vitamin D analogues:
Effective and safe in psoriasis
Main side effect is skin irritation which usually lessens with usage
Excessive use can result in systemic hypercalcaemia
Calcipotriol ointmnet (Dovonex) - once-twice/day
Also available as scalp solution
Not licensed < 6 years old
Use once to twice per day
Maximum use 100g/week
Not suitable for face as too irritating
Calcitriol (Silkis ointment) - once to twice per day
Not licensed < 12 years old
Not as irritating as calcipotriol
So more suitable for flexural and facial psoriasis
Maximum use 30g/day
Calcipotriol with Betamethasone:
Apply daily for 4 weeks
Treatment course can be repeated if necessary
Dovobet gel:
For scalp
Max 1-4g daily
Can apply to dry scalp overnight and shampoo off in morning
Dovobet ointment:
For skin
Max 15g per day
Max 30% body surface area
Enstilar foam:
Same ingredients as dovobet but studies claim that the way it is formulated it is more effective
Max 15g per day
Max 30% body surface area
2/Topical steroids:
Particulalry effective for flexural psoriasis and scalp psoriasis
Be aware of side effects with long term use
Some clinicians would hold back on prescribing potent or extra potent topical steroids (eg dermovate) on psoriatic in case it could potentially lead to a flare of pustular psoriasis on withdrawal
3/Dithranol (aka anthralin)
Can be very irritating
Unsuitable for very fair skinned patients, the face and flexures
In general the crude form is reserved for nurse led treatments in the day unit these days
At home can do “short contact” dithranol therapy: apply to patches for 10-60 minutres then wash off
Useful in resistant, localised plaques
Temporarily stains skin brown/purple/orange and can stain bed sheets/clothes so make sure patient is aware of this (ie get them to wear old pajamas and old bed sheets if using at home)
Tends to be prescribed less these days in light of advances in treatment with systemic agents
4/Coal tar
Comes in many different preparations: creams, ointments, gels, shampoos
Useful for scalp psoriasis (cocois, sebco) and chronic plaque psoriasis
Exorex is a mild preparation that the patient can use at home. Is also good for descaling plaques
Different crude coal tar regimens can be used (often nurse led in day treatment unit or as an inpatient)
Tends to be prescribed less these days in light of advances in treatment with systemic agents
Combination treatments:
Diprosalic: Salicylic acid 3% + Betamethasone
Useful for thick, hyperkeratotic scale (scalp, palms, soles)
Diprosalic solution:
For scalp
Few drops once to twice daily
Can apply overnight and shampoo off in morning
Diprosalic ointment:
For skin
Once to twice daily
Max 60g per week
Scalp psoriasis:
Thick adherent scale blocks penetrance of topical therapy
Keratolytic therapy e.g. Diprosalic can help remove scale
If have long hair advise part it and applying directly to the scalp.
Occlusion with a shower cap overnight can help soften scale
Avoid forcefully removing scale as can make it worse due to Koebner phenomenon
The BAD website skinhealthinfo.org.uk has a good video for patients on how to apply treatments in scalp psoriasis (support and resources - video guides)
Other scalp preparations:
Cocois ointment:
Coal tar 12%, Salicylic acid 2% and sulphur 4%
Good for psoriasis, seborrhoeic dermatitis and eczema of scalp where scale is thick and adherent
Rub into scalp, leave overnight with shower cap and wash off in morning
Clobetasol proprionate 0.05% (Etrivex)
• For moderate-severe scalp psoriasis
• Used if regular topical corticosteroids are not working
• Should be applied and left on for 15 minutes uncovered, and washed off
• Do not use >4 weeks at a time
Medicated shampoo preparations to wash out topical therapies include:
CapasalR shampoo
Salicylic Acid 0.5%, Coconut Oil 1%, Distilled Coal Tar 1%
Polytar shampoo
Coal Tar Solution 4%
Alphosyl 2 in 1 shampoo
Alcoholic extract of coal tar 5%
PHOTOTHERAPY
Narrowband uvb
(aka TL-01)
First line treatment
Can be whole body or localised (eg hands and feet)
Useful for chronic plaque and guttate psoriasis
Is time consuming for patient: needs to attend phototherapy service two-three times/week over a period of approx 3 months usually
Individual treatments takes up to 10 minutes
Often for approx 20-30 sessions
Often results in improvement/clearance of psoriasis for a number of months but then can often recur
Risks:
Sunburn type reactions
Photosensitive rashes: eg polymorphic light eruptions
HSV reactivation
Drug photosensitivity
Accelerated photoageing
Increased risk of skin cancer with increasing cumulative dose
Slight increased risk of cataracts
Lifetime limits:
Current recommendation is that ‘ceiling’ of treatments should be about 500 treatments (equivalent to 15-20 course)
If have had this amount of treatments they should get annual review for skin exam looking for skin lesions
PUVA
Second line
Again can be whole body or localised to hands and feet
Tends to be more effective then narrowband uvb with possible longer remission period but carries a higher risk of side effects including increased risk of skin cancer (especially SCC)
UVA is UV radiation of wavelength 320-360nm
‘P’ stands for psoralens. Psoralens make the skin temporarily sensitive to UVA allowing it to be more effective at lower doses
The psoralen can be taken orally, topically applied or mixed in a bathwater solution (often prescribed in psoriasis affecting hands and feet)
Oreal psoralens: 8-MOP or 5-MOP
Tend to give 8-MOP 2 hours prior to treatment
Eye protection must be worn for 24 hours from time of taking tablets- cataract risk
When getting treatment glasses with UVA protection should be used
If get nausea can change to 5-MOP
Lifetime limit:
‘Ceiling’ of 200 treatments recommended
Again if have had over this amount should get annual review
SYSTEMIC TREATMENT
If there is no improvement with topical treatment and phototherapy then may consider a systemic agent
NICE guidance:
Offer a systemic non-biological thrapy to people with any type of psoriasis if:
It cannot be controlled with topical therapy and
It has a significant impact on physical, psychological or social wellbeing and
1 or more following apply:
Psoriasis is extensive (eg > 10% BSA affected or PASI > 10)
Psoriasis is localised and associated with significant functional impairment and/or high level of distress (eg severe nail disease or high impact site)
Phototherapy has been ineffective, cannot be used or has resulted in rapid relapse (defined as > than 50% baseline disease severity within 3 months)
Choice of drugs:
Offer MTX as first choice of systemic agent for people who fulfill the criteria for systemic therapy and have no contraindications to it
Offer ciclosporin as first choice of systemic agent for people who fulfil the crtieria for systemic agent and who:
Need rapid or short-term disease control (eg psoriasis flare) or
Have palmoplantar pustulosis or
Are considering conception (both men and women) and need systemic therapy
Consider changing from methotrexate to ciclosporin (or vice versa) when response to first choice is inadequate
Consider acitretin for adults and in exceptional cases only for children and young people in following circumstances:
If MTX and ciclosporin are not appropriate or have failed or
For people with pustular forms of psoriasis
Regimens:
Use incremental dosing of MTX (eg start 5mg or 10mg ow) and gradually increase up to effective dose and max of 25mg per week
Assess treatment response after 3 months at target dose and stop if response is inadeaquate (eg decrease of < PASI 75 or a decrease of less than 50% PASI and 5 points in DLQI score)
Use to 2.5-3mg/kg/day of ciclosporin
Escalate to 5mg/kg/day if no response to lower dose or when rapid disease control is needed (eg severe, unstable disease)
Assess treatment response after 3 months at optimum dose of ciclosporin and stop treatment if response is inadequate
Use the lowest possible therapeutic dose of ciclosproin to maintain remission for up to 1 year
Consider other treatment if disease relapses rapidly after stopping ciclosporin (ie wiwthin 3 months)
Use incremental doses to minimise mucocutaneous side effects and achieve a target dose of 25mg daily in adults
Consider dose escalation to 50mg dailly when no other treatment options are available
Assess treatment response after 4 months at optiumum dose of acitretin and stop treatment if response is inadequate
Other medications used in psoriasis (I hope to update information regarding these in the future)
Apremilast
Skillarence (a fumaric acid ester)
BIOLOGICS
NICE/BAD criteria for use of biologics in psoriasis:
Offer biologic therapy to people with psoriasis requiring systemic therapy if methotrexate and ciclosporin have failed, are not tolerated or are contraindicated
and
The psorisis has a large impact on physical psychological or social functioning: DLQI > 10
and
One or more of the following apply:
PASI ≥ 10
BAD guidelines also include, but NICE does not:
If it is severe at localized sites and associated with significant functional impairment and/or high levels of distress (eg nail disease or high-impact difficult to treat sites - eg face, scalp, palms, soles, flexures, genital)
Consider a biologic earlier in pathway (eg if MTX has failed, not tolerated or contraindiated) in people who also have active psoriatic arthritis
You then review biologic treatment (at specified timeframe depending on the biologic agent used) and continue if there is:
A 75% reduction in PASI score (PASI 75)
or
A 50% reduction in PASI score (PASI 50) and a 5-point reduction in DLQI
The BAD has good guidelines on use of the biologics in psoraisis
In particular, the supplementary material has good information about each individual biologic agent (Much of the information below is gleaned from this) and it also has a decision aid which can be complementary to information leaflets when discussing with patients about choice of biologic to go with)
https://onlinelibrary.wiley.com/action/downloadSupplement?doi=10.1111%2Fbjd.19039&file=bjd19039-sup-0001-FileS1.pdf
The BAD also has a UK biologics checklist which outlines what should be done prior to commencing on a biologic, this includes:
Screening lab investigations:
FBC
U&E
LFT
ESR
Hepatitis B/C and HIV serology
VZV serology
ANA/dsDNA
Fasting lipids/glucose
Quantiferon test
CXR
Other important things to do:
Recommend pre-treatment flu and pneumonia vaccinations (also covid vaccines if not up to date)
Ensure cancer screening has been performed appropriate to patient’s age and gender:
Cervical screening: Every 3 years 26-49, 5 years 50-64
Breast screening: Women aged 50-70 every 3 years, over 70 self referral
Mechanism of action of biologics:
Different biologic agents exert their effects by targeting specific cytokines in the psoriasis pathway
Therefore it is useful to have a basic knowledge of the inflammatory pathways involved in psoriasis
Keratinocytes can respond to a trauma or a trigger by releasing substances that can activate dendritic cells
Dendritic cells can determine what happens to a naive T cell and push it down a particular pathway
For instance Th2 cells tend to be involved in eczema and this pathway involves IL 4 and IL 13 cytokines
In psoriasis Th1 cells and Th17 cells are the main T cells involved
Th1 pathway:
IL 12 is realeased by the dendritic cell
This activates Th1 which makes TNFa and IFNy
TNFa classically is involved in anti-tumour activity
IFNy classically is involved in fighting infections (particularly viruses)
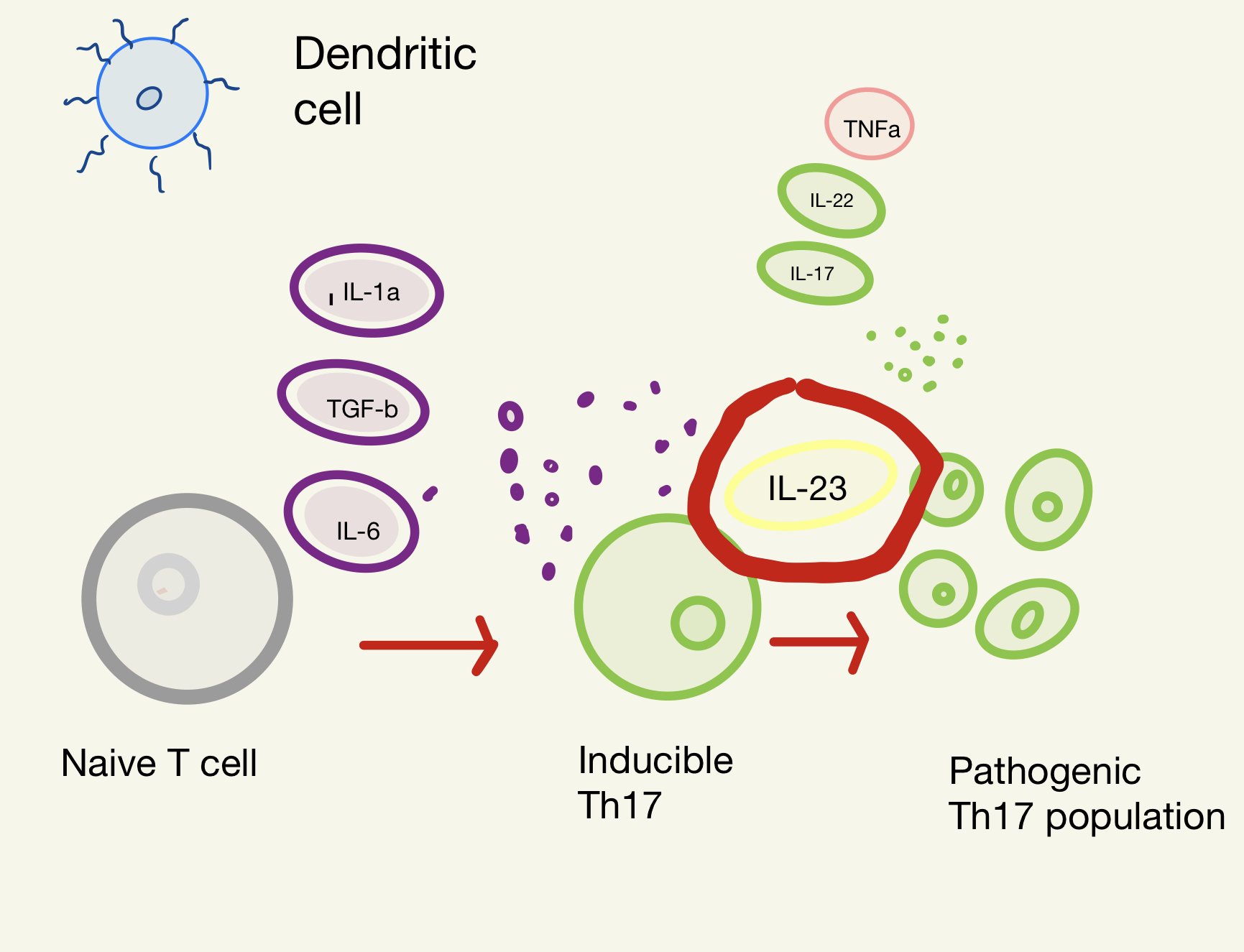
Th17 pathway:
Dendritic cells can release IL 1a, TGFb and IL-6
These turn a naive T cell into inducible Th17
Through IL-23 this becomes a pathogenic Th17 population which release IL-17, TNFa and IL-22
These damage keratinocytes which can release more substances to activate dendritic cells creating a cycle
Different biologics target different cytokines in these pathways:
Anti-TNFa agents:
Adalimumab (generally the first line biologic treatment used due to cost effectiveness)
Etanercept
Infliximab
Certolizumab
IL-12/23 inhibitors:
Ustekinumab
IL-17A inhibitors:
Secukinumab
Ixekizumab
Brodalumab (IL 17RA inhbitor)
IL-17F inhibitors:
Bimakizumab
IL-23 inhibitors (p19 subunit)
Guselkumab
Risankizumab
Tildrakizumab
ANTI TNFa AGENTS
Both Th1 and Th17 pathway lead to increased levels of TNFa
Biosimilars exist for all anti-TNFs except certolizumab
Anti-TNFs still first line due to cost effectivenesss (adlimumab primarily used, etanercept/infliximab used less often)
Usually given subcut (infliximab given IV)
Contraindicated in:
• Active TB
• History of MS/1st degree relative with MS
• NYHA III-IV heart failure
Latent TB is a relative contraindication - could potentially use one if absolutely necessary but should discuss a positive quantiferon test with an ID specialist for treatment of latent TB prior to commencing
ADALIMUMAB
Dosing:
Adalimumab: 80mg loading, 40mg at week 1 and then 40mg fortnightly
If have inadequate repsonse at 16 weeks may benefit from increasing to weekly
(Can also increase to weekly if loss of response)
Can consider MTX (if no contraindications/no prior intolerance) to prevent anti-drug antibodies
(6-50% of patients develop antibodes to adalimumab)
Children/young people:
Severe chronic plaque psoriasis in children from 4 years of age who had inadequate response or inapproprpirate for topical and phototherapies
20mg every other week (10-30kg weight)
40mg every other week (for > 30kg weight)
Evaluate response: At 16 weeks and consider stopping if not responding
Half life: Mean 14 days (range 10-20 days)
Rough proportion PASI 90 at 3- months: 41%
Likelihood of staying on it past 1 year: 77-81%
Proportion stopping due to unwanted effects:
2%
Proportion getting serious infection in first 3-4 months: < 1%
Conditions to be hesitant about:
Moderate-severe heart failure, MS (or other conditions affecting nerves)
Does if work for PsA: Recommmended treatment
CERTOLIZUMAB
Certolizumab has a unique molecular structure with no Fc region (‘pegylated’)
Therefore there there is minimal/no placental transfer of certolizumab to foetus
It is the first line biologic agent that should be used if there is intent for conception
Dosing:
Induction: 400mg (x 2 200mg subcut infections) at weeks 0, 2, 4
Maintenance: 200mg every 2 weeks
Can increase to 400mg every 2 weeks with insufficient response
Children/young people: not licensed
Evaluate response: At 16 weeks and consider stopping if not responding
Half life: 14 days approximately
Rough proportion PASI 90 at 3-4 months: 41-48%
Likelihood staying on past 1 year: unknown
Proportion stop due to unwanted effects: 2%
Proportion get serious infection first 3-4 months: < 1%
Conditions to be hesitant about: Moderate to severe heart failure, MS
Does it work for PsA: Licensed treatment
ETANERCEPT AND INFLIXIMAB
Infliximab and etanercept are not really used as much nowadays due to multiple other options
Etanercept (enbrel, benepali, erlezi)
Dosing:
50mg once weekly
Alternatively 50mg twice weekly may be used for up to 12 weeks followed by 50mg once weekly
Children and young people: From the age of 6
Children dose: 0.8mg/kg (up to max 50mg per dose) once weekly for up to 24 weeks
Evaluate response: At 12 weeks and consider stopping if no response
Half life: Mean 3 days (range 0.3 to 12.5 days)
Rough proportion PASI 90 at 3-4 months: 23%
Likelihood of staying on this past 1 year: 67-73%
Proportion stop due to unwanted effects: 2%
Proportion getting serious infection in first 3-4 months: < 1%
Conditions to be hesitant about: Moderate/severe heart failure, MS
What if I have PsA: Recommended treatment
Infliximab (remicade, inflectra, remsima, zessly, flixabi)
Higher threshold to commence as per NICE guidelines: Requires PASI > 20, DLQI > 18
Dosing:
5mg/kg given as iv infusion at week 0, week 2 and week 6
Maintenance: every 8 weeks thereafter
Children and young people: Not licensed
Evaluate response: At 10 weeks (consider stopping if no response at 14 weeks)
Half life: 8-9.5 days
Rough proportion PASI 90 at 3-4 months: 53%
Likelihood of staying on this past 1 year: 54-74%
Proportion stop due to unwanted effects: 5%
Proportioin gets serious infection in first 3-4 months: Not known
Conditions to be hesitant about: Moderaate/severe heart failure, MS
What if I have PsA: Recommended treatment
ANTI IL-12/23 AGENTS
USTEKINUMAB
(Stelara)
Ustekinumab targets the p40 subunit which is on both IL-12 and IL-23 and therefore targets both the Th1 and Th17 pathways
Dosing:
45mg (90mg if > 100kg) subcut week 0, 45mg (90mg) at week 4
Maintenance: 45mg (90mg) every 12 weeks
Children/young people: from age of 12
Children dose: <60mg: 0.75mg/kg same regime as adults
Indications to stop: Consider if poor response up to 28 weeks of treatment
NICE timelines for evaluating response to therapy: 16 weeks
Half life: Median 21 days (range 15-23 days)
Rough proportion with PASI 90 at 3-4 months: 46%
Likelihood of staying on this past 1 year: 86-92%
Proportion stop due to unwanted effects: 1%
Proportion getting serious infection in first 3-4 months: 1%
Conditions to be hesitant about: No particular condition
What if I have PsA: only whne TNFi failed
BADBIR is a registry of psoriasis patients on various systemic agents including biologic agents
Data from BADBIR is useful as it reflects real world practice with use of these agents compared to the more restricted use of agents in clinical trials
In 2015 a study looking at BADBIR data (of ustekinumab and anti-TNFa inhibitors) showed the largest proportion of patients remained on ustekinumab at 3 years followed by adalimumab, then etanercept, then infliximab
Warren R et al. Journal of Investigative Dermatology (2015). Volume 135
ANTI IL-17 AGENTS
The Th17 reponse is very important in psoraisis
IL-17A is a key cytokine involved in this pathway
SECUKINUMAB
(Cosentyx)
Dosing:
Induction: 300mg (x 2 injections) sc injection at week 0, 1, 2 and 3
Maitenance: Monthly injections starting at week 4
Children: not licensed
Indications to stop: Consider if no response up to by 16 weeks
Some with initial partial response may subsequently improve with continued treatment beyond 16 weeks
NICE timeline to evaluate response: 12 weeks
Half life: Mean 27 days (range 18-46 days)
Rough proportion PASI 90 at 3-4 months: 60%
Likelihood of staying on this past 1 year: not known
Proportion stop due to unwanted effects: 2%
Proportion getting serious infection in first 3-4 months: <1%
What are some conditions to be hesitant about: IBD, Recurrent candida
What if I have PsA: Recommended treatment
CLEAR study:
At 52 weeks secukinumab outperformed ustekinumab in multiple domains (including PASI 75, PASI 90, PASI 100 response)
Blauvelt A et al JAAD, 2017 Jan; 76 (1): 60–69
IXEKIZUMAB
(Taltz)
Dosing:
Induction:
160mg (x2 80mg injections) at week 0
then 80mg at week 2, 4, 6, 8, 10, 12
Maintenance: 80mg every 4 weeks
Children and young people: Not licensed
Indications to stop:
If have shown nor response after 16-20 weeks of treatment
If have initial partial response may subsequently improve beyond 20 weeks
NICE timelines for evaluating response to therapy: 12 weeks
Half life: Mean 13 days
Rough proportion PASI 90 at 3-4 months: 72%
Likelihood of staying on this past 1 year: Not known
What proportion stop due to unwanted effects: 3%
What proportion gets serious infection in first 3-4 months: < 1%
What are some conditions to be hesitant about: IBD, Recurrent candida
What if I have PsA: Recommended treatment
IXORA-S study:
At 52 weeks ixekizumab outperformed ustekinumab in multiple domains (including PASI 75, PASI 90, PASI 100 response)
BRODALUMAB
(Kyntheum)
Dosing:
Induction: 210mg subcut at week 0, 1 and 2
Maintenance: Then 210mg every 2 weeks
Children and young people: Not licensed
Indications to stop: Consider if show no response after 12-16 weeks of treatment
Some patients with initial partial response may subsequently improve with continued treatment beyond 16 weeks
NICE timelines for evaluating response to therapy: 12 weeks
Half life: 10.9 days
Rough proportion PASI 90 at 3-4 months: 73%
Likelihood of staying on this past 1 year: Not known
Proportion stop due to unwanted effects: 2%
Proportion gets serious infection in first 3-4 months: <1%
What are some conditions to be hesitant about: IBD, Recurrent candida infection
What if I have PsA: Not licensed
AMAGINE-2 study:
At 122 weeks brodalumab outperformed ustekinumab in multiple domains (including PASI 75, PASI 90, PASI 100 response)
So from studies it appears that IL-17 inhibition is clinically superior to both ustekinumab and anti-TNF inhibition
IL-17 INHIBITOR CONSIDERATIONS
Inflammatory bowel disease
IL-17 is important in gut inflammation
50% of patients with IBD in trials had worsening IBD
If develop lower GI symptoms on IL-17 inhibitors should screen for IBD with faecal calprotectin +/- Gastroenterologist opinion
Increased risk mucocutaneous candidiasis
Safe in latent TB
Can therefore ppotentially proceed with positive quantiferon but should speak to ID team anyway regarding whether latent TB needs treatment
?Depression
In broadlumab trial two patients had suicide and one with severe depression. When analysed was felt to be circumstantial but still could exercise caution in using these agents in people with severe depression
Psoriatic arthritis
Ixekizumab and secukinumab are also licensed for use in Psoriatic arthritis
ANTI IL-23 AGENTS
In the Th17 pathway IL-23 is upstream from IL-17
IL-23 controls the survival of pathogenic Th17 cells
The IL 23 inhibitors target the p19 subunit of IL-23
(remember ustekinumab blocks p40 which inhibits IL-12 also)
GUSELKUMAB
Dosing: 100mg sc at weeks 0 and 4
Then maintenance every 8 weeks
Children: Not licensed
Indications for stopping: Consider if no response after 16 weeks
Half life: 15–18 days
Rough proportioN with PASI 90 at 3-4 months: 68%
Likelihood of staying on this past 1 year: not known
What proportion sop due to unwanted effects: 2%
What proportioin gets serious infection in first 3-4 months: <1%
What are some conditions to be hesitant about: No conditions
What if I have PsA: Not licensed
RIZANKIZUMAB
Dosing:
Induction: 150mg (x2 75mg) sc at week 0, 4
Maintenance: Then every 12 weeks
Children: Not licensed
Evaluate: Consider stopping gf no response at 16 weeks
Some with initial partial response may improve beyond 16 weeks
Half life: Mean 28-29 days
Rough proportion PASI 90 at 3-4 months: 74%
Likelihood of staying on this past 1 year: not known
Proportion stop due to unwanted effects: 1%
Proportion getting serious infection in first 3-4 months: <1%
What are some conditions to be hesitant about: No condition
What if I have PsA: Not licensed
TILDRAKIZUMAB
(Illumetri)
Dosing:
Induction: 100mg sc at week 0 and 4
Maintenance: Then every 12 weeks
(If > 90kg: consider 200mg dosing)
In patients with some characteristics (high disease burden, body weight > 90kg,) 200mg may provide more efficacy
Children: Not licensed
Indications for stopping: if no response at 28 weeks
NICE timeline to evaluate response: 12-28 weeks
Half life: Mean 23.4 days
Rough proportion of people with PASI 90 at 3-4 months: 39%
Likelihood of staying on this past 1 year: Not known
What proportion sop due to unwanted effects: 2%
What proportioin gets serious infection in first 3-4 months: <1%
What are some conditions to be hesitant about: no condition
What if I have PsA: not licensed
BIOLOGICS: CONCEPTION, PREGNANCY AND BREASTFEEDING
Psoriasis and pregnancy:
Lots of women’s psoriasis during pregnancy goes in to remission
Remission during pregnancy associated with classical HLA-Cw6 genetic variation (approx 60% may go into remission)
Therefore some women may elect to stop treatment once they conceive
Unfortunately, patients can also have a flare, which is rarer, but not infrequent
Some registry based studies have linked particularly severe psoriasis with adverse maternal and neonatal outcomes although there are some conflicting studies on the subject
Biologics and pregnancy:
Important to advise women of childbearing potential about contraception
In women who are planning conception or are pregnant:
Counsel on importance of controlling severe or unstable psoriasis
Most pregnancies reported in women exposed to TNF antagonists at conception and/or during preganncy have sucessful outcomes with no increase in stillbirths, congenital malformations, preterm births or neonatal infections
Exposure to TNF antagonists at pregnancy may increase risk of maternal infection
Therefore patient should have all her up-to-date vaccinations or at least this should be recommended
Maternal IgG is activley transferred to foetus in 2nd and 3rd trimesters and impact of this on neonatal development and risk of infection has not been adequately studied
In general, live vaccines must be avoided for first 6 months of life in infants born to mothers taking biologic therapy beyond 16 weeks gestation
Certolizumab transfer across the placenta is low or negligible
If decision to use a systemic treatment when planning conception or during pregnancy is made:
Consider certolizumab as 1st line choice
Consider using ciclosporin or certolizumab as 1st line when necessary to start systemic agent during 2nd or 3rd trimester
Consider stopping other biologic therapy in 2nd/3rd trimester to minimize foetal exposure
Breastfeeding:
Can consider reastarting a biologic agent in women wishing to breastfeed
The small amounts of biologic therapy present in breast milk are unlikely to be absorbed systemically by infant
Males and conception:
Regarding TNFa agents there is limited evidence but this shows successful outcomes in most pregnancies with no increased risk of congenital malformations, preterm births or small for gestational age infants
IMMUNOSUPPRESSOIN AND VACCINATIONS
Live vaccines need to be avoided if you are taking immunosuppressants as taking the live vaccine can cause severe infection
General advice:
• Inactivated vaccines should ideally be given at least 2 weeks before treatment, but can be given during immune suppression treatment (may be less effective)
• Live vaccines if needed, should be given at least 4 weeks before treatment with immunosupressants is started
• Live vaccines should not be given to patients taking immune suppression treatment (specific advice for shingles vaccine)
• Live vaccination should not be given within 6-12 months of biologic treatment, 12 months of of other systemic immunosuppression (eg methotrexate, ciclosporin) or 3 months of oral prednisolone at following doses:
> 2mg/kg/day for 1 week or
>1mg/kg/day for 1 month in children or
> 40mg/day for > 1 week in adults
(Can refer to UK Green Book regarding up to date time intervals regarding this for individual agents)
Live attenuated vaccination in infants born to pregnant a women on a biologic agent:
Live attenuated vaccine should be postponed until the postnatal influence of the mother’s immunosuppressive drug treatment on the infant’s immune system has faded away
In the case of foetus exposure to TNF antagonists and other biological medicines beyond 16 weeks gestation: any live attenuated vaccination should be postpone until infant is aged 6 months old (this includes rotavirus, BCG vaccine)
Chickenpox vaccine if required:
Need to give vaccine prior to commencing a biologic agent if not immune
Vaccination involves having 2 separate injections 4 to 8 weeks apart and then need to wait further 4 weeks prior to commencing medicatoin
This may delay starting treatment for up to 3 months
If no protective antibodies and already on an immune-suppressing drug and you have any contact with chickenpox you may need an injection of chickenpox antibodies: VZIG
Shingles vaccine:
Live vaccine to prevent shingles is currently being offered to people aged 70-80 in UK
It is considered safe for patients on low dose immunosuppressive medication to receive this vaccine
PSORIATIC ARTHRITIS EXTRA
Chronic inflammatory arthritis associated with psoriatic plaques
-can involve peripheral joints, spine and/or tendons/ligments (enthesitis)
Likely that the inflammation begins in the enthesis with possibility for secondary synovitis compared to RA in which you get a primary synovitis
Many psoriasis patients can get PsA within 5-10 years of skin symptoms
Estimated 20-30% of psoriasis patient have PsA
Most (but not all) with PsA will also have psoriasis
85% will have skin disease before PsA (and can precede PsA by years - often 10 years or more)
RF PsA:
Nail psoriasis
Scalp, flexural and severe psoriasis
HLA B27 (higher for axial disease than peripheral disease)
Uveitis/IBD
Obesity
Positive family history
Structural damage can occur before appearance of clinical symptoms
Up to 50% of patients with PsA experience bone erosion in first two years after diagnosis
Once have erosions you can’t reverse this damage
Probability of achieving drug free remission has a significant negative association with a diagnostic delay of > 1 year and a significant positive association with early rheum encounter < 6 months
So there is a ‘window of opportunity’ to get disease under control early. If diagnosis is dalyed there are possible long-term consequences of decreased QOL
Therefore early identification is very important
Psoraitic arthritis is often underdiagnosed in dermatology clinics
To recognise patient who may have psoriatic arthritis think of mnemonic: DEANS
Dactylitis
Enthesitis
Arthritis (including axial arthritis)
Nail invovlement
Skin
Dactylitis:
Get red, swollen digit
Get synovitis and soft tissue oedema
More common in feet but can occur in both hands and feet
Due to inflammation of the flexure tendons (the ‘pulleys’ on both sides of the finger)
Affects approximately 50% of people with PsA
Can be acute (and painful) but can also be chronic (not painful)
So always ask if patient ever gets swollen fingers or toes
Enthesitis:
Affects up to 50% of patients with PsA
Get inflammation of insertion points of tendons, ligaments and joint capsule fibres into bones
Can get new bone formation
On exam look for pain at tendon insertion sites
Common sites of attachement of achilles tendon and plantar fascia
Also: lateral epicondyle elbow, knee
So enquire about pain under heel when walking which can become worse after period of inactivity
Also ask about pain in soles of feet
Enthesitis may be tender on palpation
Investigations:
US and MRI both good at picking up enthesitis
Arthritis:
Think of mnemonic DRAMA:
DIP predominant disease (5%)
RA like symmetric polyarthritis (15%)
Asymmetric mono/olligoarthritis (60-70%)
arthritis Mutilans (5%)
Axial arthritis (5%)
DIP arthritis:
Associated with psoriatic nail change
Inflammatory arthritis limited to DIPs
Increased frequency with disease duration
Often associated with dactylitis and nail dystrophy
If patients is < 40: inflammation of DIP joints tends to only take place in PsA
[> 40 consider gout and OA also]
RA like symmetric polyarthritis:
PIP, MCP, wrist and elbows tend to be affected
RF negative
Asymmetric mono/oligoarthritis (oligo: means 4 joints or less affected)
Commonest presentation of psoriatic arthritis
Commonly involves fingers and toes
Has predilection for DIP, PIP, ankles, knees
Arthritis Mutilans:
Most severe form. Thankfully rare.
Get a severe ostolytic disease of peripheral joints where bone is lost
Get digital shortening
May have redundant skin with shorter, wider and softer digits
Can get telescoping of digits and extreme disfigurement
Axial arthritis (resembling ankylosing spondylitis)
Can be difficult to detect clinically
Get restricted spinal movements
Can get bony ankylosis with fusing of the joints
Sacro-iliitis: Get inflammatory lower back pain with early morning stiffness
Spinal involvement: Can get cervical, thoracic or lumbar back pain
Asking about inflammatory arthritis:
Peripheral joints: Joint pain, redness, swelling. Early morning stiffness
Axial arthritis: Spinal pain and stiffness after rest. Often improves with exercise. If it gets better with rest is likely to be mechanical back pain. If worse with rest or tend to take NSAIDs in morning to help this is a good clue to inflammatory back pain
Nails:
90% of PsA patients have nail invovlement
Skin:
Have an increased risk of PsA if have severe psoriasis, scalp psoriasis and flexural psoriasis
Other associated conditions with PsA:
Uveitis: Infrequent (1-18%) of PsA patients but potentially very serious
Investigations:
PEST score:
A screening tool that can be used in the dermatology clinic
94% sensitive
Non-specific (75%) -may pick up other conditions like osteoarthritis/fibromyalgia
In general is better in younger patients but maybe not so useful in older patients
Lab investigations:
ESR/CRP (50% have elevated acute phase reactants)
RF, anti-CCP (negative)
Imaging:
X-ray hands:
Predilection for interphalangeal joints
‘Pencil in cup deformity’ (distal bone sharpened like a point)
Fusiform tissue swelling (‘sausage digit’)
Tuft resorption
Eccentric erosions
X-ray axial disease:
Erosions and sclerosis around sacroiliac joints
Fusion of spinal joints
May only affect parts of spine
Other imaging:
US - highly sensitive (can pick up inflammatory changes in joints and enthesitis)
MRI - very sensitive at detecting a sacroiliitis
Management options (driven by rheumatology)
NSAIDs unless contraindicated (with PPI cover)
Options include:
Naproxen 500mg bd (safest in older patients and patients with CV history)
Celecoxib 200mg (cox 2 inhibitor)
Etorcoxib 30-120mg od (60mg often given inflammatory arthritis)
GRAPPA (Group for research and assessment of psoriasis and psoriatic arthritis) have a suggested treatment algorithm 2021 based o type of arthritis
In general can consider:
DMARDs: Methorexate, sulfasalizine, Leflunamide
Biologics: Generally anti-TNF first, then IL-17 next, then a JAKi can be considered
Apremilast is also a possibility but probably lower on the list